Lateral luxation
Lateral luxation
Lateral luxation is the displacement of a tooth in either a palatal or a lingual direction and is almost always associated with a dento-alveolar fracture.
Clinical findings
Lateral luxation may result in:
The patient being unable to bite together
The crown is displaced palatally or lingually
The apex will move in the opposite direction
The tooth is locked into position and is firm.
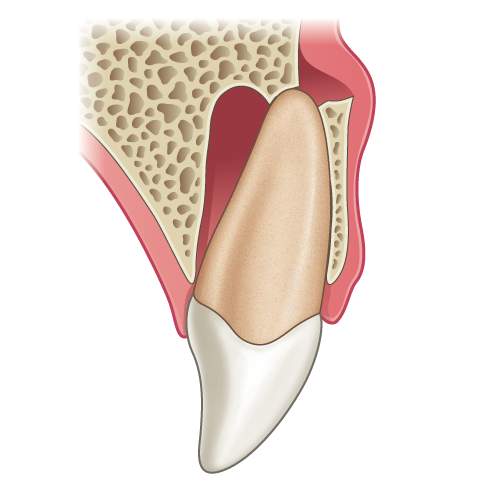
Illustration: Longitudinal section of a tooth showing a lateral luxation injury.

Clinical image: Labial view showing palatal luxation of UR1 with resultant occlusal interference.

Clinical image: Occlusal view of upper labial segment demonstrating extent of palatal luxation UR1.
Radiographic findings
Taking a good periapical radiograph of a palatally displaced tooth is difficult and the resultant image is dependent on the direction of displacement, the positioning of the film or receptor and x-ray tube. As a result a combination of:
Widening of the periodontal ligament space in some areas and
Loss of periodontal ligament space in other areas of the displaced tooth.
“With a dento-alveolar fracture the apex of the tooth can slip in front of the fractured alveolus as a result the tooth becomes locked in position and is firm, unlike in extrusion injuries. Mobility is therefore an important sign to distinguish between these two types of injuries.”
– Ms Serpil Djemal

Radiograph: Displaced UR1 showing widening of periodontal ligament space in some areas and loss in others. This radiograph demonstrates the difficulty sometimes encountered when imaging displaced teeth.
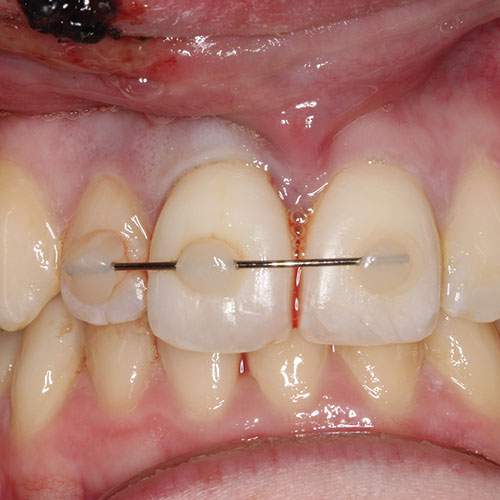
Clinical image: Labial view of UR1 following digital repositioning and splinting of the teeth with 0.016” orthodontic stainless steel wire and composite.
Management of primary teeth
No occlusal interference – allow the tooth to reposition spontaneously
Mild occlusal interference – selective grinding of the primary tooth out of traumatic occlusion can be performed
Severe occlusal interference – either attempt to reposition the tooth (being cautious of the developing permanent tooth) or consider extraction. Extraction may be under local anaesthetic or if this is not possible refer to a maxillofacial unit for extraction under GA.
Management of permanent teeth
Digitally reposition the luxated tooth under local anaesthetic
Check the occlusion (there should be contact between the posterior teeth)
Splint the tooth temporarily (on the incisal edges)
Take a check radiograph to make sure that the tooth is fully repositioned (look for a uniform periodontal ligament space around the tooth)
Once it is confirmed that the tooth is in the correct position – a flexible splint should be applied
Advise a soft diet
Advise the patient to return to normal tooth brushing as soon as possible (if there are extensive soft tissue injuries diluted chlorhexidine mouthwash can be advised for a few days)
Monitor the pulpal health at subsequent follow-up appointments and a follow-up period of 5 years is advised
Tooth discolouration soon after the injury may be transient. Patients should therefore be reassured and no diagnosis of necrosis made in the absence of any other signs or symptoms (particularly within the first three months after the injury).
Splinting
IS IT NECESSARY?
Yes splinting is necessary for cases of lateral luxation.
Splint the tooth temporarily and then ensure that the tooth has been repositioned correctly by taking a radiograph.
Then apply a flexible splint.
SPLINTING TIME
The recommended time for splinting in lateral luxation is 4 weeks.
WHAT MATERIALS TO USE?
Several different materials are available for splinting a 0.016″ stainless steel orthodontic wire with composite resin.
This should be extended to one uninjured tooth either side of the injured teeth.
Monitoring: The pulpal response should be monitored at subsequent appointments and a follow-up period of 5 years is advised.




